The published study focuses specifically on Barrett’s Esophagus (BE), the only known precursor to esophageal adenocarcinoma (EAC). Despite causing few symptoms, BE is considered a precancerous condition, with patients who have dysplastic BE being at a higher risk of developing EAC. This type of cancer is challenging to detect in its early stages and is often misdiagnosed during endoscopic screening and surveillance. The prognosis for EAC is currently poor, with only 20% of patients surviving beyond five years. Given the limited tools for detecting BE and EAC and its association with such a deadly form of cancer, research into early detection and timely treatment is crucial.
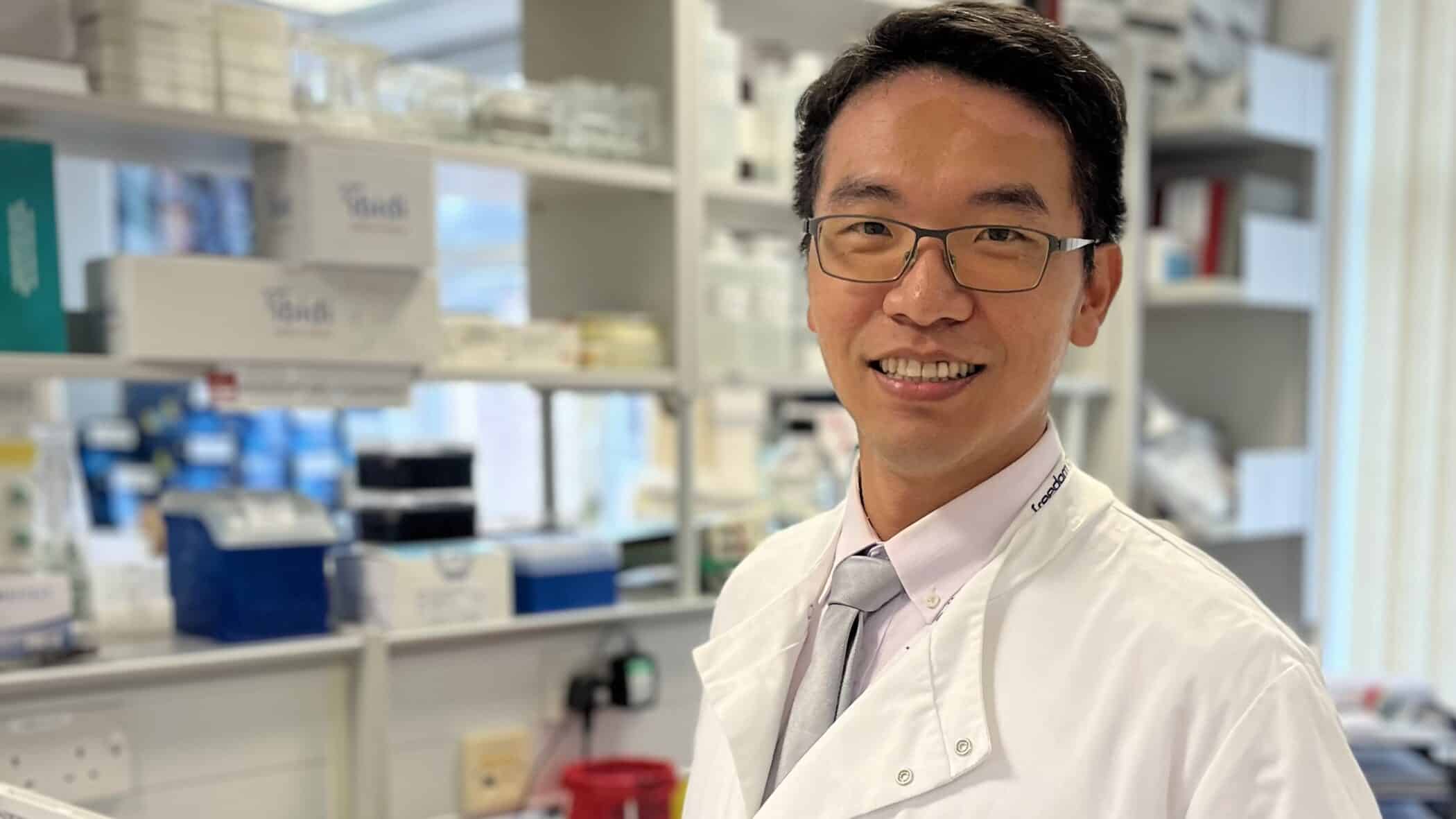
Yi-Jhih is part of a team, headed by Professor Katherine Vallis, that recognises the importance of advancing understanding in this area and has recently published a study demonstrating the application and use of the endoscopic detection platform – fluorescence molecular endoscopy (FME) – by ‘EMI-137’ in preclinical animal model with early and dysplastic BE. Summarizing the study and its findings, Yi-Jhih explains:
“This research paper explores the use of EMI-137, a c-MET-specific peptide labelled with a near-infrared fluorescent dye (Cy5**), as a tool for detecting dysplastic lesions in BE…the real-time FME demonstrated that the EMI-137 fluorescence signal presented a positive correlation with the degree of dysplasia. This study suggests that EMI-137 has the potential to serve as a novel tool for dysplastic BE lesions identification, aiding in the early detection of cancerous changes in BE patients and providing more accurate endoscopic examinations and treatments.”
With such positive results, Yi-Jhih and their team’s research suggests important developments in the detection and treatment of EAC and significantly advances the limited knowledge around the disease.
The full study can be found here.